There is no explanation for why cancer mortality rates have not gone down (and have gone up) despite medical advances as the entire nation has stopped smoking. Investment in screening and treatment can ensure near 100% recovery, yet all budgeting goes to cheaper "prevention" which does not work. Since the US cracked down on tobacco use, with success in white males, the overall cancer mortality rate has increased from 184 per 100,000 in 1950-69 to 209 per 100,000 from 1970-1994. Today that rate holds steady at 203 per 100,000. In white females and in other demographics cancer mortality rates have been steady or changed in negligible amounts, but these demographics have had increasing tobacco use rates. Cancer is a painful and unnatural death that can often involve long battles with the disease and should be combatted with all resources available, in treatment and in prevention. While lung cancer rates have fallen, technological advances have allowed earlier detection of lung cancer, which at stages 0 and 1 is among the least deadly forms of cancer, but at later stages is among the most deadly. Without adjustments for technological advances in medical care, no positive statement can be made in regards to success or negative results from anti-smoking campaigns. Meta-data from overall cancer mortality does show that the resources in the war on cancer have been squandered and had an overall detrimental effect on the national health of the country, and some policy change is necessitated, although it must be noted there is no current biological explanation for the lower cancer rates in countries and places with higher tobacco use, these have been correlative not causal links. Atmospheric nuclear weapons testing does match up with the population data, it was ended by the 1970's with the Limited Test Ban, and in the continental USA in 1962, and there is solid science that shows inhaled radioactive particles cause lung and other cancer for 30-60 years after detonation.
See cancer rates in USA: http://ratecalc.cancer.gov/ratecalc/archivedatlas/pdfs/maps/acc-maps.pdf
It can also be noted that the demographic distribution provided in the atlas is vitally important as the female population increased smoking rates slightly and saw a slight decrease in cancer mortality as well as an increase in life expectancy commensurate with the increases seen before anti-smoking campaigns.
Please note that the modern terminology for measuring radiation exposure is the gray which measures radioactive exposure per kilogram of tissue, as opposed to the rad which was formerly used and is an absolute amount of radioactive exposure. In humans, one gray is equal to about 100 rads.
According to mapping of fallout from nuclear weapon's testing the majority of the southern states in the USA are exposed annually to an average of over 1 rad of radiation, from fallout alone, exposure to this level of radiation (lifetime of around 100 rads) radiation results in a, "decrease in the circulating white cells and platelets." This results in a statistically significant increase in cancer in keeping with the findings shown on this atlas as, "The Biologic Effects of Ionizing Radiation report (BEIR V) states that if 100,000 people are exposed to 10 rads of radiation, then there will be 800 additional cancers in that population above the normally occurring amount." Source: http://cancernews.com/data/Article/264.asp#sthash.qEIXcULD.dpuf
We can expect cancer rates to drop significantly as the average radiation exposure in the USA has dropped since this map was made in 1997, the current average annual exposure is still .6 rads per year, enough that there are a significant number of people with lifetime exposure exceeding 100 rads.
Source: http://www.epa.gov/rpdweb00/understand/calculate.html
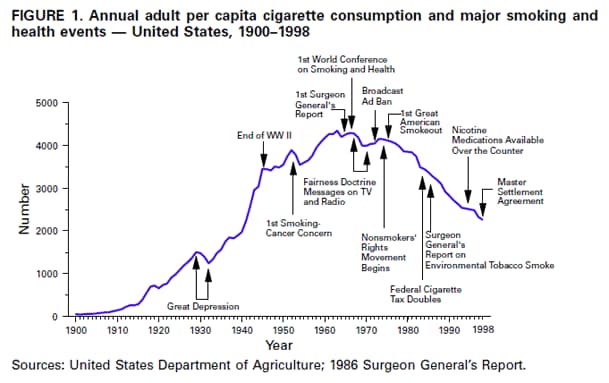
Finally, a primary concern of smoking (though the claim asserted by anti-smoking campaigns is that it increases all forms of cancer), has been lung cancer. This disease takes on average 20-30 years to develop (Howlander et al.), and while cigarette consumption had reached 80% and 90% of its peak by 1945 and 1950, respectively, lung cancer peaked in 1991 and 80% and 90% were reached in 1973 and 1980, respectively. Most importantly there are no spikes and dips as with tobacco use rates and consumption, but lung cancer is a smooth increase and decline, in direct communication with radioactive exposure and pursuant half-lives. Lung cancer mortality has not decreased in kind with decreasing smoking rates however, and in fact only plateaus with the ban of nuclear weapon's testing and nuclear power plant construction. While cigarette smoking has dropped by over half since 1975, lung cancer mortality has gone from 75 to 65 per 100,000, an insignificant change which after adjusting for atmospheric radiation actually indicates that smoking cessation has cost many lives. See image below for lung cancer mortality in the USA.
Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975–2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/browse_csr.php?sectionSEL=15&pageSEL=sect_15_table.19.html, based on November 2013 SEER data submission, posted to the SEER Web site, April 2014.
LAFUMA, J., CHMELEVSKY, D., CHAMEAUD, J., MORIN, M., MASSE, R., AND KELLERER, A. M. Lung Carcinomas in Sprague-Dawley Rats after Exposure to Low Doses of y Rays. Radiat. Res. 118, 230-245 (1989).
National Cancer Institute at the National Institutes of Health
See cancer rates in USA: http://ratecalc.cancer.gov/ratecalc/archivedatlas/pdfs/maps/acc-maps.pdf
It can also be noted that the demographic distribution provided in the atlas is vitally important as the female population increased smoking rates slightly and saw a slight decrease in cancer mortality as well as an increase in life expectancy commensurate with the increases seen before anti-smoking campaigns.
Please note that the modern terminology for measuring radiation exposure is the gray which measures radioactive exposure per kilogram of tissue, as opposed to the rad which was formerly used and is an absolute amount of radioactive exposure. In humans, one gray is equal to about 100 rads.
Study Estimating Thyroid Doses of I-131 Received by Americans From Nevada Atmospheric Nuclear Bomb Test, National Cancer Institute (1997)
Annual dose in rads
Annual dose in rads
It can be seen above that the white and light blue areas of dangerous levels of radiation (previously believed that 2 rads annually were safe, now it is known that virtually no level of radioactive exposure is safe) matches smoking data exactly (as shown below, and later in the article). Cancer mortality on the other hand, has changed drastically as far as geographic distribution over the years. According to research done on rats, lung cancer can be induced in significant amounts with any amount of radiation, and differences between groups exposed to 1 gray of radiation (100 rads) can be seen to be at least 13 times greater than in control groups (LaFuma et al.).
According to mapping of fallout from nuclear weapon's testing the majority of the southern states in the USA are exposed annually to an average of over 1 rad of radiation, from fallout alone, exposure to this level of radiation (lifetime of around 100 rads) radiation results in a, "decrease in the circulating white cells and platelets." This results in a statistically significant increase in cancer in keeping with the findings shown on this atlas as, "The Biologic Effects of Ionizing Radiation report (BEIR V) states that if 100,000 people are exposed to 10 rads of radiation, then there will be 800 additional cancers in that population above the normally occurring amount." Source: http://cancernews.com/data/Article/264.asp#sthash.qEIXcULD.dpuf
We can expect cancer rates to drop significantly as the average radiation exposure in the USA has dropped since this map was made in 1997, the current average annual exposure is still .6 rads per year, enough that there are a significant number of people with lifetime exposure exceeding 100 rads.
Source: http://www.epa.gov/rpdweb00/understand/calculate.html
Finally, a primary concern of smoking (though the claim asserted by anti-smoking campaigns is that it increases all forms of cancer), has been lung cancer. This disease takes on average 20-30 years to develop (Howlander et al.), and while cigarette consumption had reached 80% and 90% of its peak by 1945 and 1950, respectively, lung cancer peaked in 1991 and 80% and 90% were reached in 1973 and 1980, respectively. Most importantly there are no spikes and dips as with tobacco use rates and consumption, but lung cancer is a smooth increase and decline, in direct communication with radioactive exposure and pursuant half-lives. Lung cancer mortality has not decreased in kind with decreasing smoking rates however, and in fact only plateaus with the ban of nuclear weapon's testing and nuclear power plant construction. While cigarette smoking has dropped by over half since 1975, lung cancer mortality has gone from 75 to 65 per 100,000, an insignificant change which after adjusting for atmospheric radiation actually indicates that smoking cessation has cost many lives. See image below for lung cancer mortality in the USA.
A doctor I interviewed on this matter mentioned to me that it was a possibility that infectious diseases were accountable for the increase in cancer mortality, but that they did not know for certain, not having looked these statistics up. I have acquired the infectious disease mortality rate, and it has not changed since anti-smoking campaigns went into effect and in fact increased which means that the potential positive effects of tobacco may be even greater than suggested by simply looking at other raw data, possibly due to lost funding diverted to misguided anti-smoking campaigns. In any case the veracity of the failure of anti-smoking campaigns cannot be questioned in the war on cancer, and is a monumental public policy choice that must be reverted immediately.
Works and Sources Cited:
Centers For Disease Control
Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975–2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/browse_csr.php?sectionSEL=15&pageSEL=sect_15_table.19.html, based on November 2013 SEER data submission, posted to the SEER Web site, April 2014.
LAFUMA, J., CHMELEVSKY, D., CHAMEAUD, J., MORIN, M., MASSE, R., AND KELLERER, A. M. Lung Carcinomas in Sprague-Dawley Rats after Exposure to Low Doses of y Rays. Radiat. Res. 118, 230-245 (1989).
National Cancer Institute at the National Institutes of Health




No comments:
Post a Comment